Tracking health threats, one sewage sample at a time

A sewage treatment plant in Norfolk, Va., is one of the sites where workers collect wastewater samples to test for COVID trends in the nearby community.
Meredith Rizzo/NPR
hide caption
toggle caption
Meredith Rizzo/NPR

A sewage treatment plant in Norfolk, Va., is one of the sites where workers collect wastewater samples to test for COVID trends in the nearby community.
Meredith Rizzo/NPR
VIRGINIA BEACH, Va. – The best time of day to collect a wastewater sample is in the morning. That’s according to Raul Gonzalez, an environmental scientist who’s an expert on how people’s hygiene habits intersect with the flow of sewage.
Gonzalez runs the wastewater surveillance program at the Hampton Roads Sanitation District, a Virginia Beach, Va., sewage treatment operation that processes waste for 20% of the state’s population. He and his team were early adopters of wastewater surveillance – a way of tracking the concentration of viruses, bacteria and infectious diseases in sewage to watch for infectious disease outbreaks.
Since March 2020 – months before the Centers for Disease Control and Prevention launched a national initiative – Gonzalez and his colleagues have been tracking COVID levels in the sewage that comes through their plants.

Wastewater — from nearby homes, businesses, toilets and sinks — ends up at the Virginia Initiative Plant in Norfolk, Va., where it gets routed through various stages of treatment before being released into the Chesapeake Bay.
Meredith Rizzo/NPR
hide caption
toggle caption
Meredith Rizzo/NPR

Wastewater — from nearby homes, businesses, toilets and sinks — ends up at the Virginia Initiative Plant in Norfolk, Va., where it gets routed through various stages of treatment before being released into the Chesapeake Bay.
Meredith Rizzo/NPR

Notes
Wastewater oxidizes in one of the tanks at the treatment facility.
Wastewater data is a useful complement to the traditional metrics of cases, hospitalizations and deaths, health experts say. The data don’t depend on people seeking out testing or labs reporting results. Instead, it relies on people’s daily habits, and the fact that people carrying the virus will shed it when they poop. It identifies broad trends quickly, and can be used to test for other pathogens like flu, polio, mpox and antibiotic-resistant bacteria.
How wastewater surveillance happens
How does a piece of the virus that causes COVID from someone’s gut flow from their toilet to the sewage treatment plant — and end up as a data point on a COVID dashboard? At the Hampton Roads Sanitation District, it takes two days and the labor of many people. It all starts with a sample gathered early in the day, to catch people’s morning poops.

Marcos Davila-Banrey and Jon Nelson prepare to capture a wastewater sample for the Hampton Roads Sanitation District COVID surveillance program.
Meredith Rizzo/NPR
hide caption
toggle caption
Meredith Rizzo/NPR

Marcos Davila-Banrey and Jon Nelson prepare to capture a wastewater sample for the Hampton Roads Sanitation District COVID surveillance program.
Meredith Rizzo/NPR

Nelson lifts a sterile plastic bottle at the end of a pole filled with murky wastewater. The water sample he retrieves will become useful information on the levels of COVID in the nearby community.
Meredith Rizzo/NPR
hide caption
toggle caption
Meredith Rizzo/NPR
On a recent, gray day at a treatment plant in Norfolk, Gonzalez’s colleague Jon Nelson stood over a small metal hatch that opened onto a pipe of incoming sewage. He put a sterile plastic bottle at the end of a long pole more typically used to hold a paint roller, and lowered it about 18 feet into the river of wastewater coming from the region’s homes, campuses and businesses.
By the time it gets to the plant, sewage smells just a little sulfurous and it’s not brown, but a murky gray. “It looks nothing like what you see in the toilet,” says Joshua Coyle, an operations lead at the plant – in the journey through the pipes, “[the fecal matter] all dissolves and breaks down.”

Once the wastewater is bottled, it becomes a precious sample. It’s chilled in a cooler of ice, to keep it fresh for the 20-minute drive to the labs at the sewage utility’s headquarters.
It’s a ritual the team has conducted every week for the past three years – not just at this one plant but at the eight they manage, covering 5,000 square miles in southeast Virginia.

Raul Gonzalez, at a Hampton Road Sanitation District lab in Virginia Beach, Va. He leads the district’s wastewater surveillance program which began monitoring COVID levels in March 2020.
Meredith Rizzo/NPR
hide caption
toggle caption
Meredith Rizzo/NPR
The program took a lot of “blood, sweat and tears” to stand up, Gonzalez says, recalling the early, uncertain days of the COVID pandemic and the experimentation it took to find reliable ways to measure COVID in the wastewater. Now, they’ve got their process dialed in.
Cleaning up sewage samples back in the lab
At the sewage utility headquarters, the sample passes through three adjacent laboratories and several staff to get the virus filtered out of the sewage water, cleaned and then counted.

Notes
When the wastewater arrives at the lab, acid is added to positively charge virus particles in the sample.

Kat Yetka (left) pours the wastewater sample over a filter (right), negatively-charged to better capture COVID virus particles, at a Hampton Road Sanitation District lab in Virginia Beach, Va.
Meredith Rizzo/NPR
hide caption
toggle caption
Meredith Rizzo/NPR
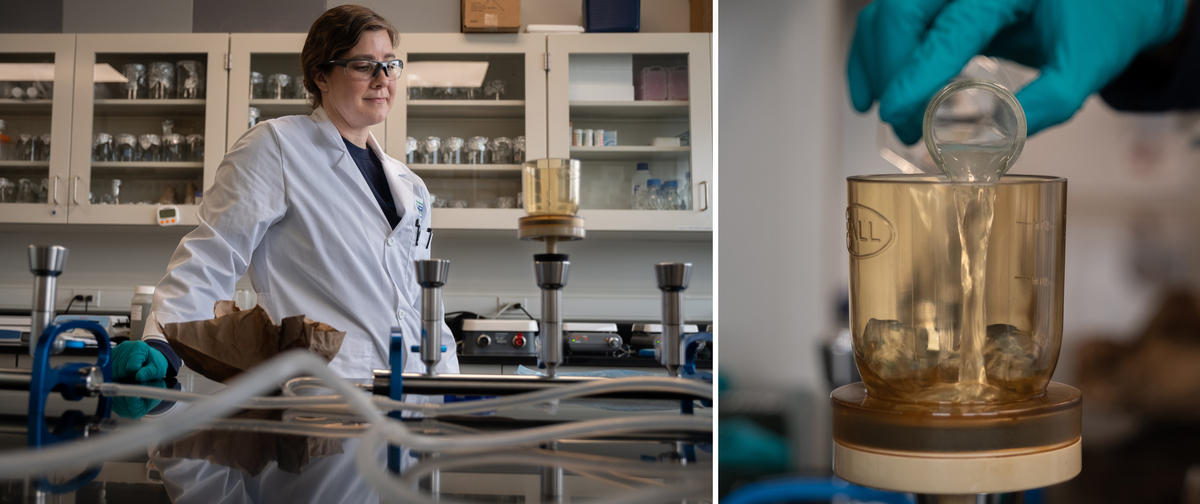
Kat Yetka (left) pours the wastewater sample over a filter (right), negatively-charged to better capture COVID virus particles, at a Hampton Road Sanitation District lab in Virginia Beach, Va.
Meredith Rizzo/NPR
The first step is to pass some of the liquid from the bottle through a paper filter, which helps separate the virus from the sludge in the water. Staff scientist Kat Yetka adds acid to the sample to positively charge the virus particles, so they’re more likely to stick to the negatively-charged filter. It takes just a few minutes. The sample has gone from a one-liter bottle of liquid, to a small paper filter, about the width of an Oreo cookie. Yetka folds it with forceps and sticks it in a test tube.
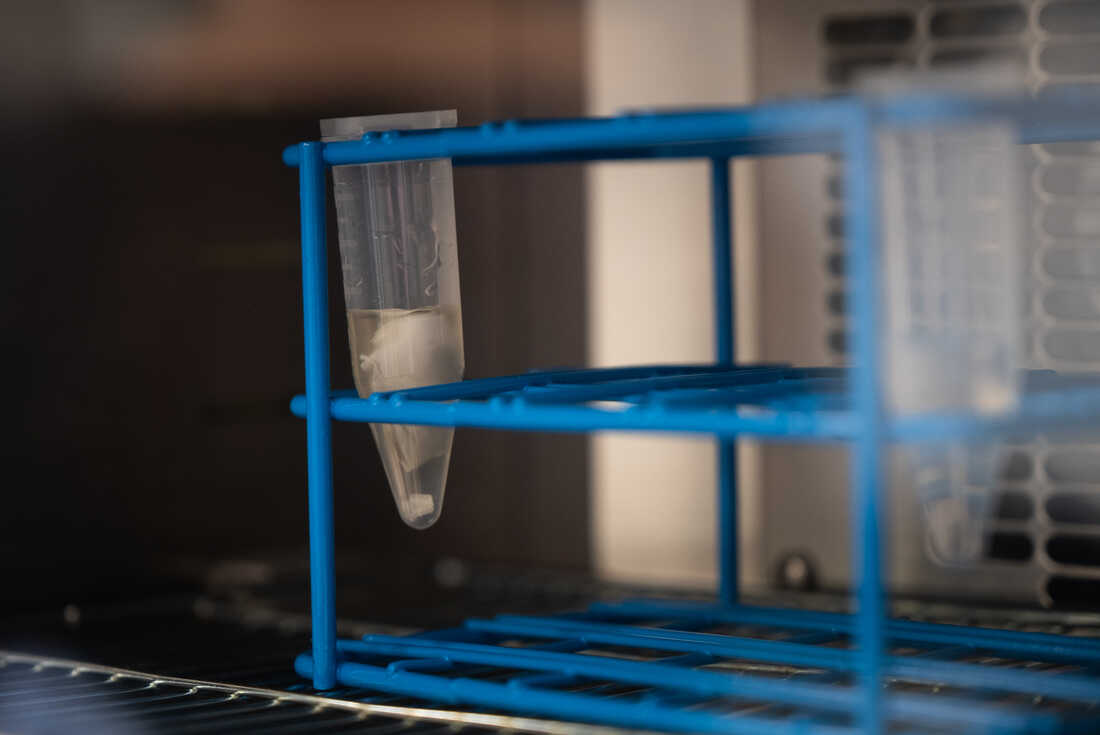
The filter soaks in a small vial as part of the process.
Meredith Rizzo/NPR
hide caption
toggle caption
Meredith Rizzo/NPR

The filter soaks in a small vial as part of the process.
Meredith Rizzo/NPR
That filter gets bathed in chemicals to release the viral RNA from cells in the sample, and then to wash away poop and other detritus. “[We’re washing] everything from solids to organic materials to salts out of the sample,” Gonzalez says, “We’re trying to clean up everything but the targets we’re looking for.”
Once the sample is as clean as it’s going to be — it’s time to start quantifying how much virus the researchers have collected.
Hannah Thompson, a microbiologist at the lab, adds a fluorescent dye to the sample, which glows when it attaches to the COVID virus. She takes a bit of the treated liquid — about the size of a raindrop — and breaks it down into many smaller droplets. It’s the ratio – of droplets that have COVID in them, versus those that don’t – that will serve as the basis for figuring out how much virus is in the total sample.
She then puts the droplets into a machine that makes copies of the virus’ genetic code “through 40 cycles of heating and cooling, heating and cooling” she says, so the levels will be high enough to measure.
“By the end, we’ll have billions of copies,” Thompson says. The process takes several hours, so they set it to run overnight.
Hannah Thompson mixes probes and primers that she adds to the sample to help identify COVID in the water. The goal is to run these through a machine that will amplify any COVID in the liquid.
Meredith Rizzo/NPR
hide caption
toggle caption
Meredith Rizzo/NPR
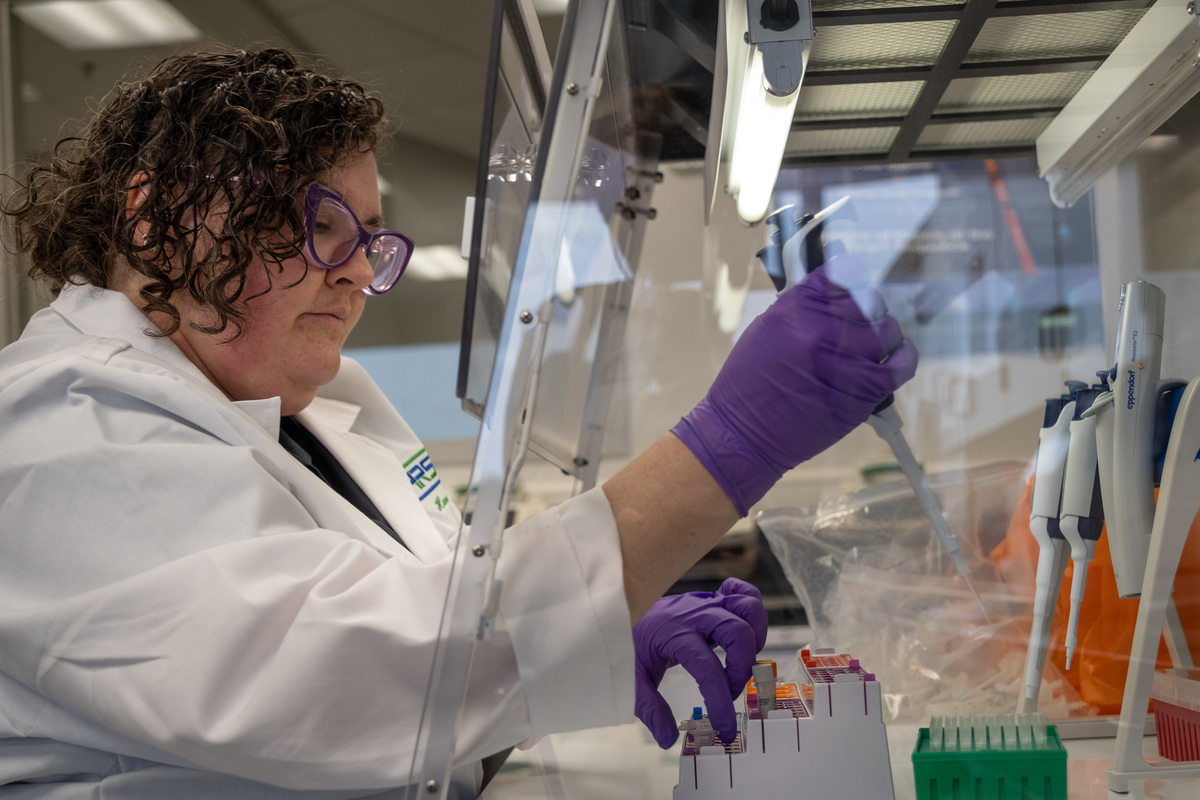
Hannah Thompson mixes probes and primers that she adds to the sample to help identify COVID in the water. The goal is to run these through a machine that will amplify any COVID in the liquid.
Meredith Rizzo/NPR
Here in Virginia Beach, processing a single wastewater sample takes two days and multiple skilled workers. This isn’t the process everywhere – some sewage plants collect samples that they then send off to state health departments or the CDC’s federal contractors to process.
And many plants don’t participate at all – it’s completely voluntary. The CDC says that nationally, the wastewater surveillance program they coordinate covers around 40% of the U.S. population.
In addition to analyzing their own wastewater, Gonzalez’s team also sends some samples to Virginia’s health department and the CDC. Still, he says his team is continuing its own efforts in-house because it creates a consistent record dating back to the start of the pandemic, and it’s useful for their local health departments.

Early the next morning, Gonzalez is back at the lab with Hila Stephens, a molecular biologist, who runs the plate with the droplets through a machine to figure out how much COVID was in the sample.
“I’m betting my money on a trend that’s been going for awhile,” Stephens says, “So there’ll be some COVID in the water.” She is right. The amount of COVID in the water that week in March is about the same as it was the week before.
The sewage data drives a public health dashboard
The data gets shared on a public dashboard. Kyle Curtis, Gonzalez’s fellow environmental scientist on staff, runs the numbers through a computer script to visualize how the levels are trending. Even though the virus level are high (as of this reading in March), hospitalizations and deaths are as low as they’ve been this whole pandemic.
“I think we look at it with different eyes than we used to,” Curtis says. “In previous waves, we didn’t know what the ceiling [of infections and serious illness] looked like for the community.” Now, the broad level of immunity from vaccinations and previous infections means that high levels of COVID don’t necessarily forecast many COVID deaths.
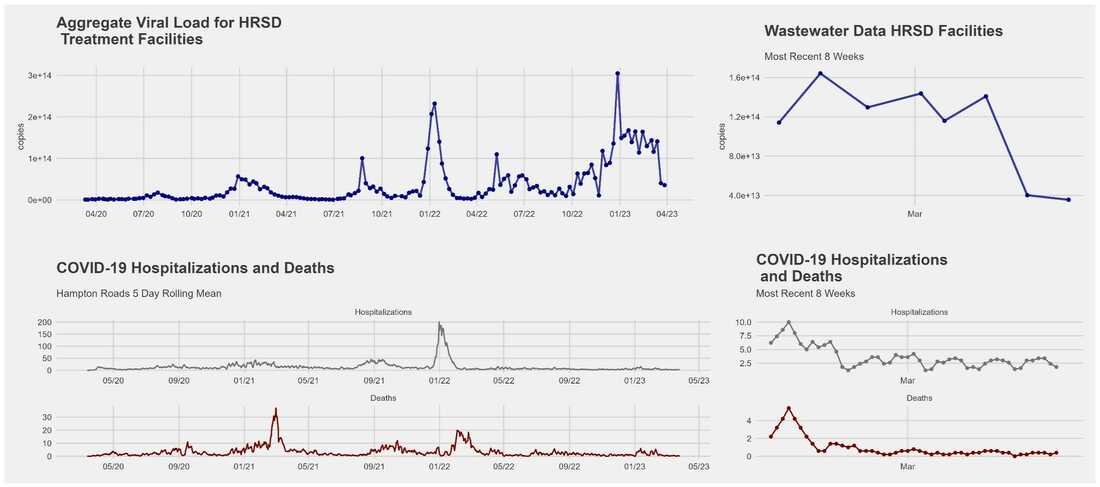
Gonzalez and his team use the surveillance data they collect to track overall trends in COVID infections. The information is made available on a public dashboard alongside hospitalizations and deaths in order to give a fuller picture of the health of the community.
HRSD/Screenshot by NPR
hide caption
toggle caption
HRSD/Screenshot by NPR
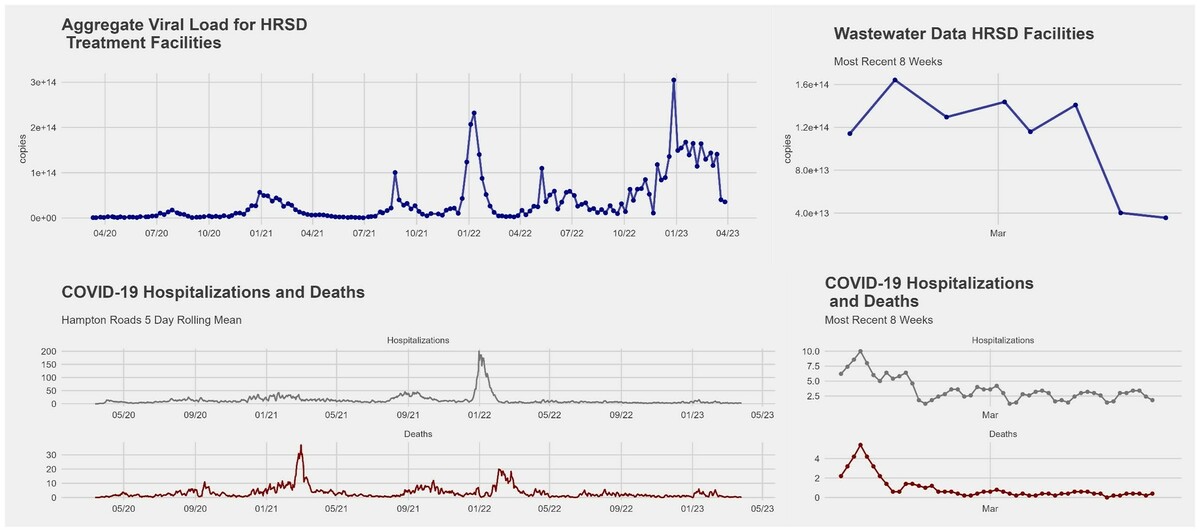
Gonzalez and his team use the surveillance data they collect to track overall trends in COVID infections. The information is made available on a public dashboard alongside hospitalizations and deaths in order to give a fuller picture of the health of the community.
HRSD/Screenshot by NPR
Still, public health officials say these trends are important to track.
“None of these single data points are perfect,” says Dr. Caitlin Pedati, head of the Virginia Beach Department of Public Health. “But if I look at my wastewater trends together with hospitalization data and what’s going on in nursing homes, among high-risk facilities and populations, that’s going to give me a decent sense of whether activity is going up, going down or staying the same.”
That in turn could be used to help her determine where and when to offer COVID testing or vaccine clinics for people at higher risk from COVID.
Wastewater surveillance got a lot of attention and funding during COVID. Many public health officials hope that’s just the start. “We’re in the process of expanding [wastewater surveillance] to a whole suite of other pathogens, from influenza and RSV to norovirus and E. coli,” says Amy Kirby, who leads the CDC’s national wastewater surveillance program.
She envisions a future where the data serve as an early warning for public health officials, and as a “health weather report” for communities, where people could check a dashboard displaying pathogen trends in their area, and use it to decide whether to wear a mask, or take precautions while traveling, or to take extra care cooking their food or washing their hands.
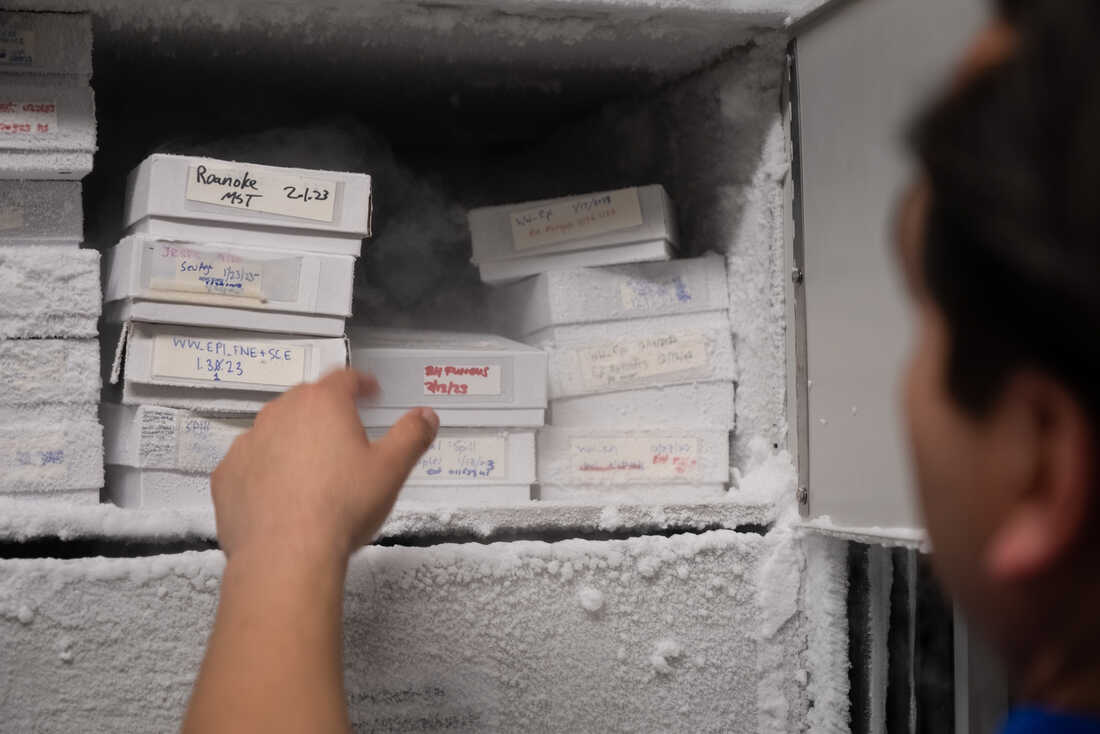
Gonzalez’s team stores a small portion of their wastewater samples in the freezer. Many public health officials hope that the attention and funding for COVID surveillance ultimately extends to other pathogens too, like tracking RSV or norovirus infections.
Meredith Rizzo/NPR
hide caption
toggle caption
Meredith Rizzo/NPR

Gonzalez’s team stores a small portion of their wastewater samples in the freezer. Many public health officials hope that the attention and funding for COVID surveillance ultimately extends to other pathogens too, like tracking RSV or norovirus infections.
Meredith Rizzo/NPR
But Gonzalez says it takes a lot of time and resources to keep it going. He’s part of a committee at the National Academies of Sciences, Engineering, and Medicine urging more funding for the national program. So far, the federal government has spent $300 million on wastewater surveillance, and is committed to spending another $320 million to expand the program through 2025.
The system could serve as an early warning signal in a future pandemic. “We’ve invested a lot to build this system, and it would be difficult to shut it down and start it up again,” Kirby says, “It’s much more cost-efficient to keep it running.” But, she says, it requires continued investment to make that real.
Photography and visuals production by Meredith Rizzo. Editing by Scott Hensley.

For all the latest Health News Click Here
For the latest news and updates, follow us on Google News.

