Mpox still circulating more than you’d think, from hot spot in Mexico to cluster of cases in Canada | CBC News
This is an excerpt from Second Opinion, an analysis of health and medical science news emailed to subscribers weekly. If you haven’t subscribed, you can do that by clicking here.
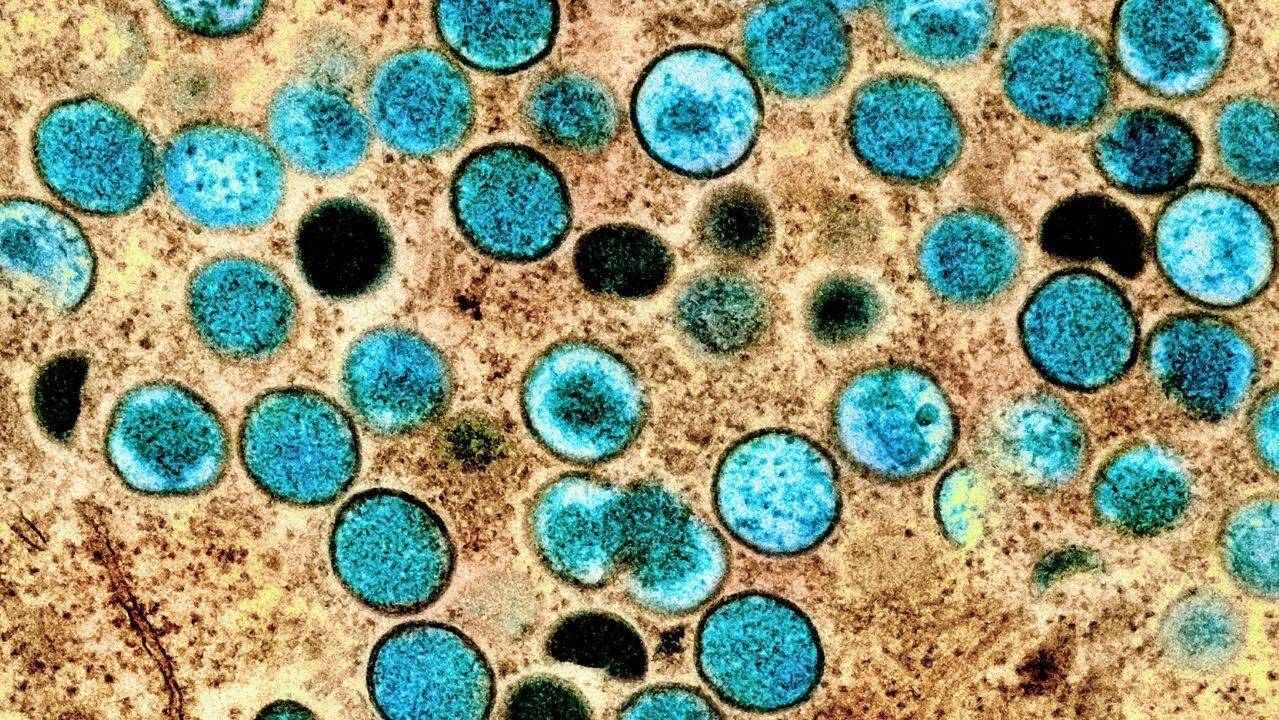
After an unprecedented global outbreak of mpox made headlines last summer, prompting awareness campaigns and widespread vaccination efforts, the virus appeared to fade away.
Cases dropped. Media coverage dried up.
So did interest in vaccines.
In Toronto, one of the key cities impacted during Canada’s months-long outbreak, public health data shows only 15 per cent of people who received a first dose have since completed the full series of shots.
Then, in January, a wake-up call in that same city: Four cases of the painful illness previously known as monkeypox were reported in just a 24-hour span. Toronto’s public health unit later told CBC News all the recent cases were “locally acquired,” rather than linked to travel abroad.
A virus forgotten, perhaps — but not gone.
“There’s still some ongoing transmission,” said Dr. Zain Chagla, an infectious diseases specialist and McMaster University associate professor. “Unfortunately, I think we probably are dealing with this in the short-term future, and probably even for some time.”
It’s no surprise, then, that the World Health Organization (WHO) made the call this week to maintain mpox as a public health emergency of international concern — and later noted the number of new cases reported globally increased by 70 per cent from the week before.
Canada’s cluster of cases offers a reminder the virus is still here, circulating to some degree. The situation elsewhere is worse. And the concern going forward is that this virus will continue popping up in new populations, striking the vulnerable all while vaccination uptake is dwindling.
“We can’t get lulled into this sense of comfortability,” said mpox researcher Jason Kindrachuk, a microbiologist at the University of Manitoba and Canada Research Chair for emerging viruses.
“Yes, we’ve gotten things contained … but we have to appreciate the virus hasn’t disappeared.”

‘Who knows’ what summer will bring
The latest WHO report showed the number of reported cases has steadily declined worldwide, yet more than 30 countries still continue to report new infections. Deaths also continue ticking up, including at least two in the U.S. so far this month.
“Even for the countries [like the U.S.] that have declared, essentially, victory … it’s important to remain vigilant,” said Dr. Boghuma Titanji, a physician-scientist at Emory University in Atlanta. “Cases are not down to zero — so who knows what the summer will bring.”
Overseas travel in the months ahead remains a concern for Dane Griffiths, director of the Ontario-based Gay Men’s Sexual Health Alliance, given the ongoing outbreaks abroad.
The highest confirmed case increase is in Mexico, with roughly 60 new infections since early February — and more than 3,800 in total — in a country that hasn’t rolled out any mpox vaccines.
“Mexico doesn’t have access to the vaccine and has a higher burden of infections. People should know that, they should understand the local outbreaks where they’re travelling to,” Griffiths said.
WATCH | What it’s like to recover from mpox:
A Toronto resident shares his experience recovering from monkeypox, while officials and advocates say more support is needed for patients during the long weeks of isolation.
The worldwide case tally is almost surely an undercount, given limited surveillance in many regions around the world. Global efforts to track mpox have slowed, the WHO warned in a recent report, and the “true burden of mpox remains unknown in most African countries.”
Canada’s first-ever outbreak of mpox exploded last summer, and there have been close to 1,500 known cases since then, largely among the men who have sex with men community — a group overwhelmingly impacted by the virus, which spreads rapidly through sexual networks.
The WHO is also calling on countries to work toward the elimination of the virus — by interrupting transmission chains, and containing any outbreaks — as much as possible.
It’s no easy feat, given the virus’ global reach and an untold number of animal hosts capable of silently housing the virus. But it’s a goal that feels vital given the debilitating pain some people experience during an active infection, and the risk of death in people who are more vulnerable to serious illness, including anyone immunocompromised.
A new study out of Belgium, published on Thursday in Eurosurveillance, also noted the potential for lingering symptoms, even weeks after an infection.
“Most importantly, clinicians should be aware of the pain, scarring and mental health issues that may persist after a seemingly self-limiting illness,” the authors wrote.
Vaccine access, uptake remain concerns
Alongside access to diagnostics and treatments, vaccination programs remain a key piece of the puzzle for tackling mpox going forward, the WHO has said.
But plenty of countries, including those in Africa, still lack access. And even in global cities that experienced major outbreaks last summer, and procured an abundance of shots — like Toronto and New York — uptake for second doses has fallen off a cliff.
“Coverage for second doses was definitely lower than we would have liked,” Griffiths, in Ontario, said. “I think that in part is the sense of urgency changing for folks, which makes sense. We went through a couple months of low or no reported cases.”

It’s also not clear just how long immunity lasts after one or two rounds of the Jynneos mpox shots.
Smallpox vaccines, which did provide some crossover protection against mpox, definitely waned over time, which may have left more people vulnerable to mpox in the first place — particularly since the shots haven’t been routinely used in Canada, or many other countries, for several decades.
And, like other vaccines, the mpox shots aren’t 100 per cent effective.
“There will always be breakthrough cases… we can’t let anyone have sort of false assurance that, ‘Oh, you’re vaccinated, you’re all good’ — because they may still contract the infection,” warned Dr. Rosamund Lewis, the WHO’s technical lead for mpox, in a call with CBC News.
More infections among women
As vaccination efforts continue, the WHO stressed that, at a global level, community transmission of mpox continues to occur particularly among “vulnerable populations of gay and bisexual men and other men who have sex with men.”
People living with HIV infections make up roughly half of all cases, and are also at risk of more severe disease.
Yet, as the worldwide outbreak ballooned, eventually hitting more than 85,000 known cases and more than 90 deaths across 110 countries, there was also an increase in the proportion of cases in women and children — showing this virus’ ability to strike broader networks of individuals, when given the opportunity.
Data shows the proportion of women getting infected globally remains under 10 per cent, but did double over the course of the outbreak, Lewis said.
It could be due to more broad transmission in African countries where the virus has circulated longer, she suggested, or may be a reflection of more trans or non-binary women getting infected.
WATCH | Mpox cases rose in Canada in 2022:
As cases of monkeypox climb in Canada, there are growing concerns that the vaccine is not widely available, and time may be running out to contain the spread.
Canadian data shows the bulk of mpox infections so far are among adults, mostly those 18 to 49, but there have also been a handful of cases among kids and teens.
The virus largely spread globally through sexual contact, but it’s long been known mpox can also transit in other settings, through close skin-to-skin contact in households or by touching contaminated fabrics or surfaces.
A case study from a tattoo parlour in Spain, published in January in the New England Journal of Medicine, showed that during one particular period, 36 per cent of customers — most of whom were female — became infected, while nearly all the piercing and tattooing items tested came back positive for the virus.
Though concerning, those kinds of situations are “often dead-end events” where there’s no onward transmission into the broader community, Chagla stressed.
Still, it’s “not a space we can ignore,” Lewis said, “because the fraction has been creeping up.”

Researchers watching for adaptations
It’s also critical, scientists say, to track the ongoing evolution of this virus — and to watch for adaptations that make it capable of sparking ongoing outbreaks among humans.
Researchers from the U.S. National Institutes of Health recently developed a mouse model to study mpox virulence. To their surprise, the Clade IIb virus — the strain behind the global outbreak — was much less severe than historic clades of this virus.
The results, the researchers say, suggest the virus is evolving to either become less severe, or adapting to better infect other species.
Titanji said no modelling study is a perfect representation of what’s happening in the real world, though this one does align with evidence already showing Clade IIb is a less virulent strain.
“The more it circulates in humans,” she added, “there is a real possibility it will better adapt to transmit human-to-human.”
The good news? The world has the tools to clamp down on transmission whenever cases do emerge, from vaccines to therapeutics — if we act fast and use them.
“Flare-ups are unfortunately common with a number of different infectious disease outbreaks,” Kindrachuk said.
“But we at least have some control over the extent of what those flare-ups will look like.”
For all the latest World News Click Here
For the latest news and updates, follow us on Google News.