Developing new nanoparticle treatments for brain tumors
Northwestern Medicine investigators have developed a novel nanoparticle treatment for glioblastoma, according to a study published in Nature Communications.
Glioblastoma, the most common type of primary brain cancer, is one of the most complex, deadly and treatment-resistant cancers, according to the National Brain Tumor Society. The five-year survival rate for glioblastoma patients hovers near 7% and has remained unchanged for decades.
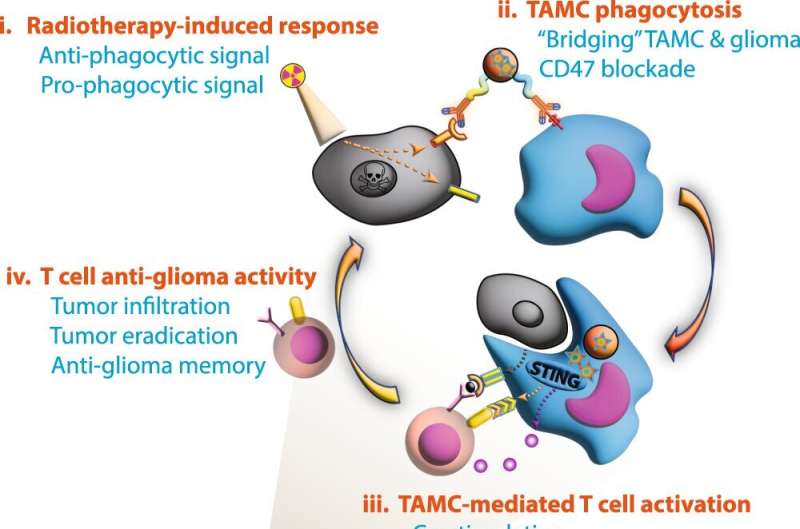
Previous Northwestern Medicine research has shown that glioblastoma tumors accumulate large numbers of immunosuppressive tumor-associated myeloid cells (TAMCs), which impairs the immune system’s ability to fight the tumor and reduces the effectiveness of radiation and chemotherapy.
“Immunosuppression is a hallmark of the tumor microenvironment,” said Peng Zhang, Ph.D., assistant professor of Neurological Surgery and first author of the study. “TAMCs are a key driver of immunosuppression and therapy resistance. Because TAMCs compose 30% to 50% of the brain tumor mass, there’s an urgent need to develop new therapeutic strategies to target and modulate those immunosuppressive cells in brain tumors.”
In the current study, investigators targeted cultured TAMCs with a nanoparticle they developed to deliver dimeric amidobenzimidazole, or diABZI, a recently developed synthetic compound which targets a protein known as stimulator of interferon genes, or STING. The nanoparticle was also loaded with antibodies targeting CD47 and PD-L1, two immune checkpoint proteins that are overexpressed in glioblastoma tumors and TAMCs after radiotherapy.
According to the study, the TAMCs that received the treatment produced markedly less immunosuppressive proteins and increased immunostimulatory proteins.
When mice with glioblastoma were treated with nanoparticles, scientists observed a spike in the number of activated T-cells, which are usually responsible for mounting an immune response against the tumor but are largely absent in brain tumors. The T-cells in the treated mice infiltrated the tumor in higher numbers and extended the lifespan of the mice, according to the study.
Additionally, tumors were eradicated in nearly 70% of the animals following the nanoparticle treatment and radiation therapy, a standard treatment for glioblastoma.
“Overcoming tumor immunosuppression is key to designing effective immunotherapeutic strategies,” said Maciej Lesniak, MD, chair and the Michael J. Marchese Professor of Neurosurgery and senior author of the study. “This approach opens the way for modulating the tumor microenvironment in such a way as to enhance the potential of immunotherapy.”
Investigators then replicated the experiment using tumor and blood samples from glioblastoma patients and again observed the reprogrammed TAMCs and activated anti-tumor T-cells.
The results suggest that the nanoparticle treatment could be an effective way to complement existing care and boost immune responses in glioblastoma, Lesniak said.
Lesniak, Zhang and their collaborators hope to bring the nanoparticle treatment to clinical trials, Zhang said.
“We also would like to gain more insight into how the host immune response could contribute to the therapy efficacy or therapy resistance of those tumors,” Zhang said. “We also want to incorporate the immune metabolism and bioinformatics into our multi-disciplinary research so we can do a thorough job regarding the design of the next generation of therapeutics against brain tumors.”
More information:
Peng Zhang et al, STING agonist-loaded, CD47/PD-L1-targeting nanoparticles potentiate antitumor immunity and radiotherapy for glioblastoma, Nature Communications (2023). DOI: 10.1038/s41467-023-37328-9
Citation:
Developing new nanoparticle treatments for brain tumors (2023, June 7)
retrieved 7 June 2023
from https://phys.org/news/2023-06-nanoparticle-treatments-brain-tumors.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.
For all the latest Science News Click Here
For the latest news and updates, follow us on Google News.

